Laser Analgesia in Restorative Applications: Is It All Just Hype?
 How many of us have heard the claims from the manufacturers stating, “Buy our laser and you won’t need to use local anesthesia again for your restorative procedures”? And how many of us bought into these claims, but were then disappointed when a patient stopped the cavity preparation, requesting that conventional anesthesia be administered, due to pain? If the claim of ‘laser analgesia’ was the main reason for such a big investment, how disappointing it is to now have such a valuable piece of equipment sitting idle in the corner of your operatory?
How many of us have heard the claims from the manufacturers stating, “Buy our laser and you won’t need to use local anesthesia again for your restorative procedures”? And how many of us bought into these claims, but were then disappointed when a patient stopped the cavity preparation, requesting that conventional anesthesia be administered, due to pain? If the claim of ‘laser analgesia’ was the main reason for such a big investment, how disappointing it is to now have such a valuable piece of equipment sitting idle in the corner of your operatory?
It is important to clarify some of the misconceptions, so then, hopefully, you can take that laser out of the corner and put it to good use, albeit with more realistic expectations. You will not be disappointed again!
There are two aspects which must be looked at when considering laser analgesia:
- Laser Pre-conditioning with red and infrared (NIR) diode laser wavelengths which takes about 2-3 min before commencing a restorative procedure. One must then use the conventional drill and burr, or a hard/all tissue laser system, such as Er:YAG 2940nm, Er,Cr:YSGG 2780nm, or CO2 9300nm for cavity preparation.
- Laser Ablation of the carious lesion with hard/all tissue laser without any pre-conditioning. The drill is only used for verification of the hardness of the remaining tooth structure (spoon excavator or a small round burr in slow speed handpiece) and to shape and polish the newly placed composite restoration.
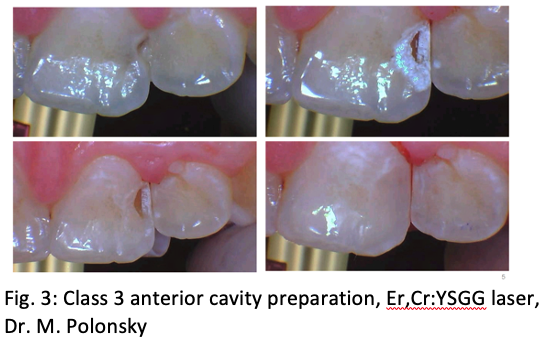
If we look at the available research regarding laser anesthesia/analgesia, it is all derived from studying red and NIR diode lasers, with wavelengths between 600-900nm. These wavelengths have deeper penetration for both soft and hard tissues, as compared to, for example, Erbium lasers, due to significantly lower absorption in water and hydroxyapatite (HA), which are the main components of gingiva, tooth, and bone respectively. When applied at the CEJ, and near the apex of the tooth, diode lasers have an excellent chance of reaching the pulp in the middle of the tooth to affect the nerve. At the ALD meeting in 2014, Dr. Gerry Ross presented his study on pre-conditioning with red 660nm and NIR 808nm diode lasers: they both delivered the same dose of 25J/cm2, and with similar outcome, as approximately 80% of 100 patients reported no pain (VAS=0) during drill cavity preparation which followed his pre-conditioning protocol (Fig. 1,2). In 2017, a split-mouth, randomized crossover clinical pilot study on 24 patients (Efthymiou et al.) was published in Lasers in Dental Science, which showed no difference in Frankl’s behaviour scale between the lased group, when pre-conditioned for 2 minutes with 810nm diode laser, and the control group given an injection of local anesthetic. This suggests that photo-bio-modulation (PBM) induced pulpal anesthesia similar to conventional anesthetic injection.
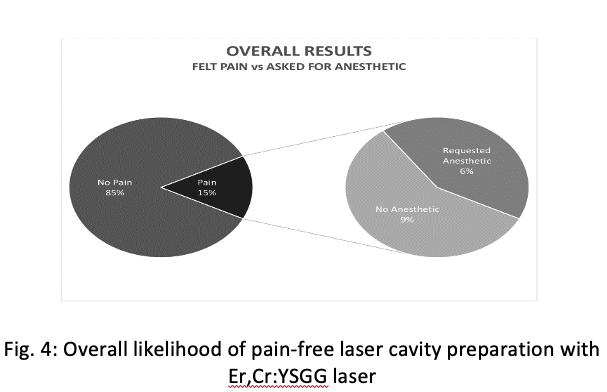
Paradoxically, it is not the diode lasers which use laser analgesia for marketing claims, but rather the hard/all tissue lasers, such as mid-infrared (MIR) Er:YAG 2940nm and Er,Cr:YSGG 2780nm, and far infrared (FIR) CO2 9300nm. These systems are able to ablate enamel and decayed dentin due to preferential absorption in tissues with higher water content; gross decay can be as high as 54% water content, by volume, compared to only 12% in healthy enamel, and 20% in healthy dentin/cementum. Clinically, we see improved patient experience due to the following: substantial reduction of vibration and drill noise; minimally invasive cavity preparation with reduced post-operative sensitivity; lack of smear layer and surface bacterial decontamination; and faster dentin bridge formation following accidental pulp exposure in deep carious lesions (Fig. 3). All these benefits from hard tissue laser cavity preparations are well documented and supported by the literature. Although, MIR and FIR laser manufacturers claim the same analgesia benefits, which we do witness clinically, the assumption that all lasers have the same mechanism for laser analgesia is incorrect. It is physically impossible for the MIR and FIR laser energy to reach the pulp, no matter how long one hovers over the tooth in an attempt to pre-condition. Presently, no research is available into the proposed mechanism of action of MIR and FIR lasers and how cavity ablation causes temporary analgesia/anesthesia.
From the many PBM studies carried out by Roberta Chow, Tiina Karu and Ambrose Chan, we have learned much about the actions of diode lasers in analgesia, however, the precise mechanism is still not well understood. We know of the neuro-pharmacologic effects on synthesis and metabolism of neurotransmitters, such as Serotonin and Acetylcholine at the central level, and Histamine and Prostaglandin at the peripheral level, as well as the upregulation of Endorphin synthesis and downregulation of Bradykinin and Substance P. Furthermore, we are also aware of the destabilizing effects on the neuronal membranes of c-fibers, which conduct pain signals to the brain, leading to altered thresholds for action potentials, as well as the effects on the axonal microtubular network inhibiting the propagation of the action potentials from one neuron to another.
The more we understand how diode laser pre-conditioning works, the more we realize that we DO NOT know how MIR and FIR lasers cause their analgesic effect, which we DO see clinically. The mechanism must be different, because the depth of penetration of MIR and FIR lasers in hard and soft tissues is measured in microns, not millimeters, so there is no possible way for these wavelengths to affect the nerves of the pulp directly through the absorption of their energy. When we consider the possible photo-biological effects being thermal, chemical, acoustic, fluorescence and bio-stimulation, the only one likely to work from a distance, with these free running pulsed laser systems, is photo-acoustic effect. Is it not possible that the same cavitation forces and shock waves, responsible for removing smear layer inside a root canal system, can also destabilize neuronal membranes and the Na/K channels long enough to complete the cavity preparation without conventional anesthesia? If we know that we are seeing laser analgesia with cavity preparations clinically, then it should be just a matter of time for the researchers to come up with a plausible mechanism of action to describe what is really happening on the neuronal level. However, this laser analgesia/anesthesia is not seen 100% of the time, with all types of patients, and with all types of cavity preparations. If it was 100% successful, we would not have any disappointed laser owners, and in fact, laser cavity preparation would revolutionize the world of restorative dentistry.
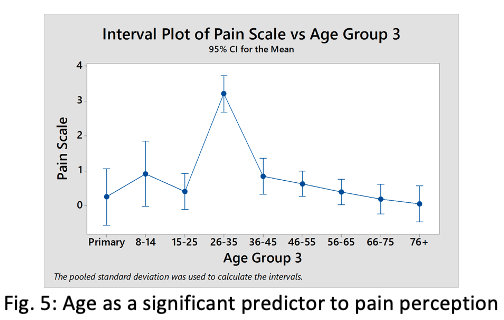
For now, we must rely on statistical interpretations of hundreds of clinical results, which have some predictive value to help with proper case selection, to ensure the best possible outcome for both the dentists’ ability to complete the laser cavity preparation, and the patient to not feel the need to stop the procedure because of intra-operative pain. In a 2017 study, by Polonsky et al., the possible pain predictors using Er,Cr:YSGG system was published in Lasers in Dental Science. It showed that in non-anxious patients, who were willing to try the laser cavity preparation without first receiving an injection of local anesthetic, 85% experienced no pain, and 9% did not experience enough to request conventional anesthesia before continuing and completing the cavity preparation. Only 6% of the 400 patients in the study felt pain to a degree which necessitated the conventional injection (Fig.4).
Some of the parameters with positive predictive values included the power settings used, Class of cavity preparation, anterior vs. posterior location of the tooth and, of particular interest, the age of the patient (Fig.5)
In conclusion, both laser analgesia and laser restorative dentistry must be investigated further, both separately and together, to support and explain with research what we, as clinicians, see in our practices. The possible synergistic relationship between red or NIR diode laser pre-conditioning, followed by laser cavity preparations using MIR or FIR laser systems, must also be considered and researched. I believe that the future of laser dentistry is bright, but no single laser system can accomplish everything, and combining wavelengths may be the key to success in achieving our ultimate goals.