- Home
- About ALD
- ALD 2024
- Education
- Membership
- Resources
- Blog
- Find A Dentist
|
ALD IMPACT REPORT
ALD CORPORATE MEMBERS
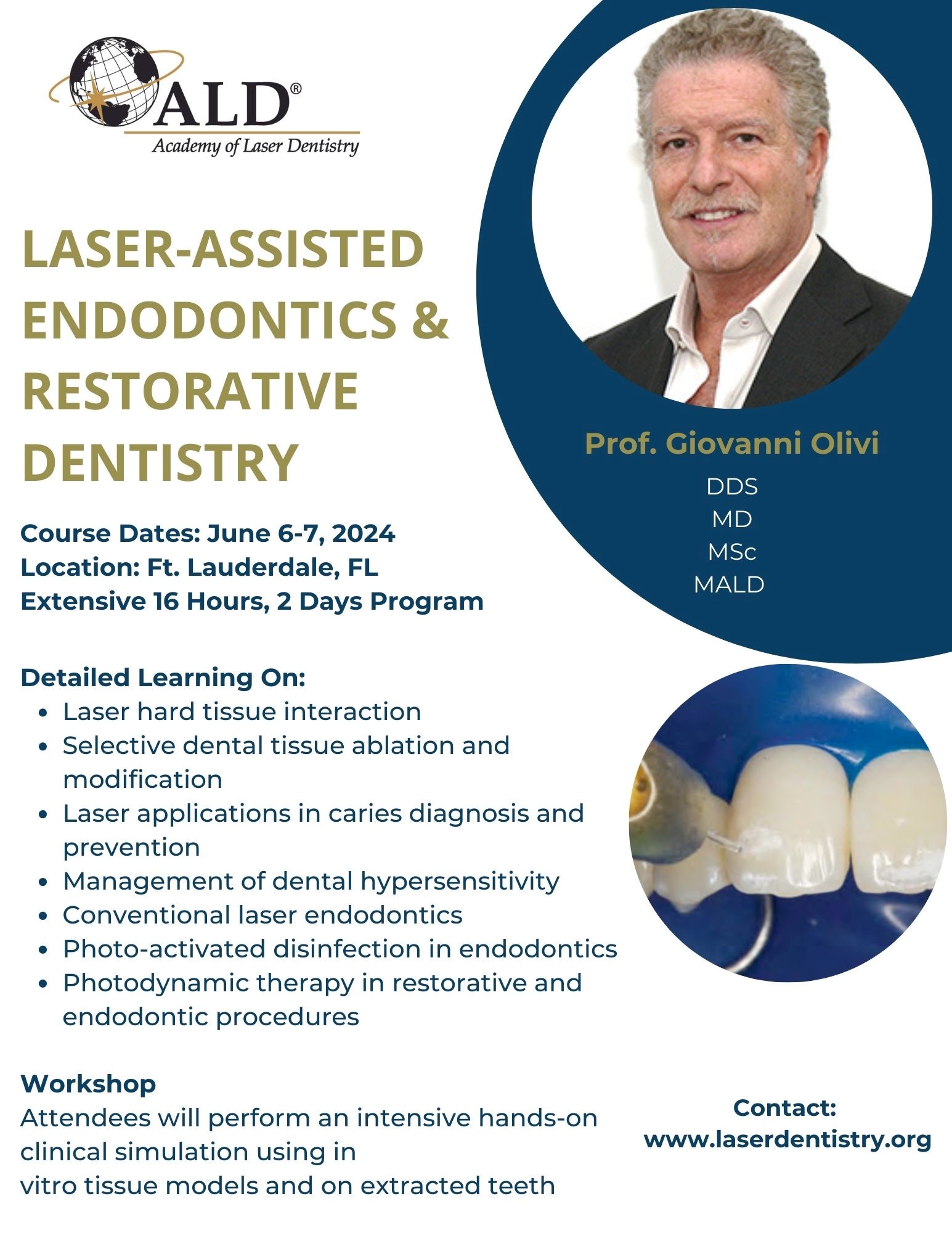
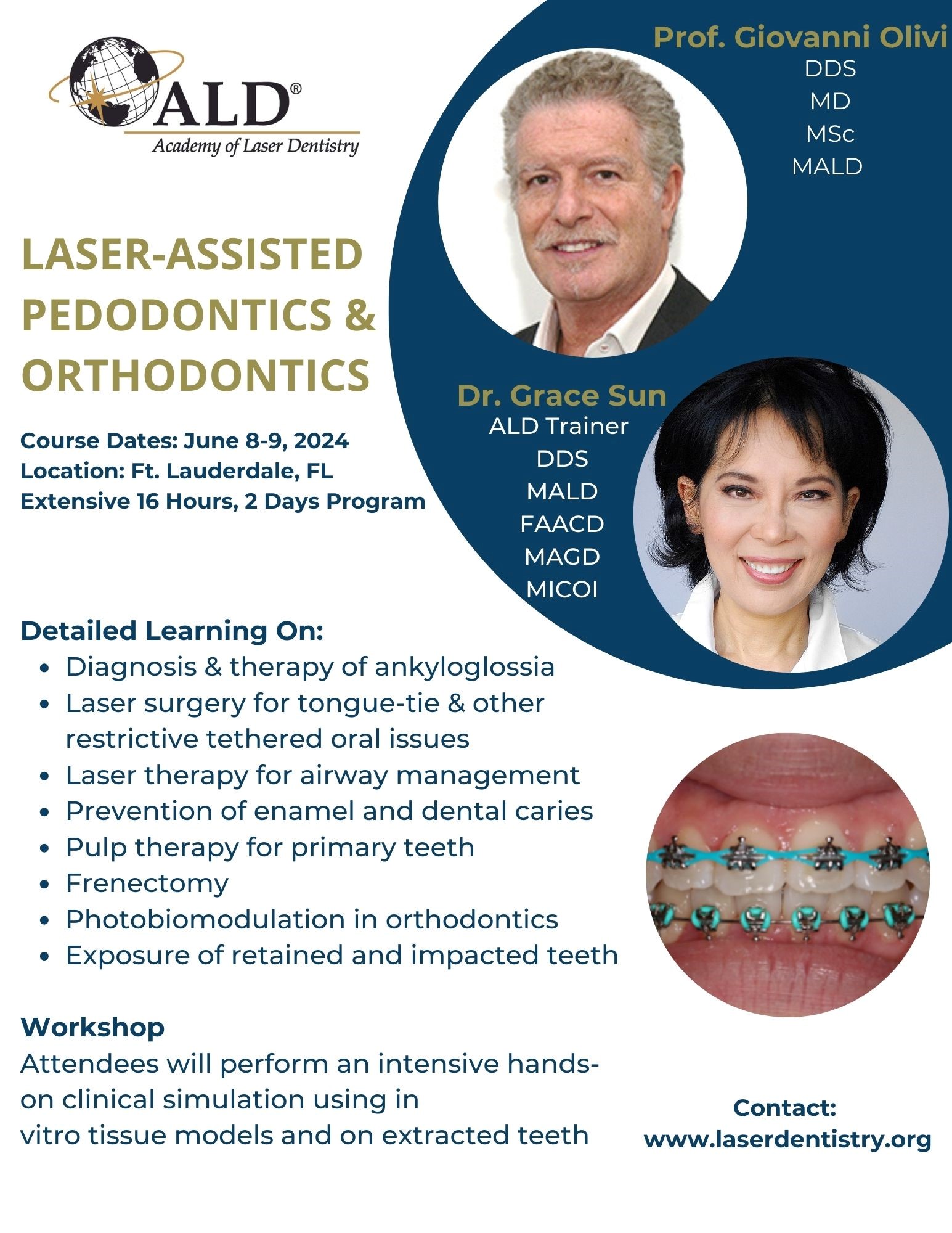
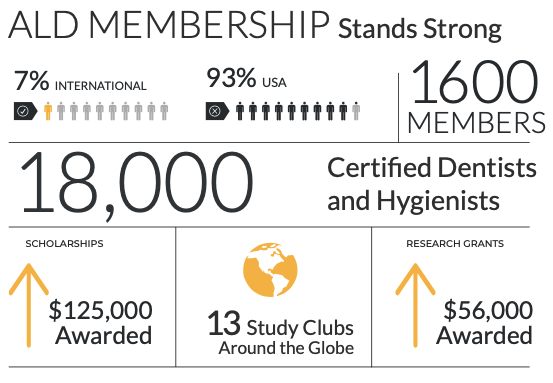
The Benefits of MembershipThrough ALD members have access to comprehensive world-class clinical education, research and practice guidance for the safe and effective use of laser technology that ensures both your patients’ and your practice’s well-being, every day. ALD Membership helps you improve laser skills, elevate your patient care, increase patient satisfaction. Successful laser practice integration provides greater profitability and insights into new laser opportunities.
Join Today
What is ALD's Laser Certification Program?The Academy of Laser Dentistry's Certification Program is a structured educational mechanism for dental practitioners wishing to demonstrate high standards and clinical proficiency in laser dentistry. Becoming an Academy of Laser Dentistry certified professional can help you differentiate yourself from your competitors, attract and win new patients, build loyalty and improve patient and team satisfaction.
CERTIFICATION FAQs |











 .
.